Anatomy of a Cough: Learn What Muscles are Affected by Respiratory Distress, Asthma Attacks, and GERD. TMJ Pain, Neck Pain, Rib Pain, and Pelvic Floor Pain are Related to Lung Distress. Learn How.
- Tara Lee Clasen

- Aug 6, 2025
- 17 min read
Updated: Dec 1, 2025

Right after finishing a post on the scalene muscles (front neck muscles), a woman emailed about needing to come in for neck and jaw pain. She had been struggling with her lungs, having asthma attacks, and had just had a “big one” a few days prior. That night, she had intense jaw tension—which is why she emailed seeking therapy. After a night's sleep, her jaw felt better, but she still had a general sense of all-over tension and neck pain.
During our session, to reverse the muscular effects of the cough, we focused on the front body: anterior (front) muscles of the neck, chest, the diaphragm, and psoas. In this post, we will touch on the main areas of tension created by a repetitive and forceful cough.
What constitutes the anatomy of an asthma or coughing attack?
Anyone who has ever had a coughing fit knows you can feel it all over—from the top to the bottom of the spine. And the tension can seem to concentrate wherever you already have tension. If the back of your shoulders were already hurting, a coughing fit stresses the ribcage, neck muscles, and shoulder muscles, exacerbating your current condition.
There are muscles that are directly affected by coughing, which when stressed, trigger pain elsewhere in the body. As you will read below, coughing affects the psoas muscle, and a stressed psoas can mask as low back pain and eventually psoas dysfunction causes addtional dysfunction throughout the low back, causing more low back pain. The psoas isn’t just stressed by coughing; it is also stressed by sitting at a desk and repetitive hip movements such as running and cycling.
A psoas that is already under stress, that is subjected to the physcial motions of respiratory distress, will gather more stress. Months later, when nagging low back pain will not go away, or when sitting at the desk seems even more uncomfortable, we may not connect it to our respiratory illness or asthma attacks.
To keep healthy, we should—in real time—consider what muscles are being overloaded. That helps us to prevent pain or to understand and holistically heal our current pain.
If you have had an acute respiratory illness, such as COVID, pneumonia, or just a cold with a bad cough, or a chronic respiratory illness, asthma, allergies, or throat irritating GERD, do a self-check-in with the muscles mentioned in this post.
KEEP READING to learn about how chronic respiratory illness can lead to kyphosis, “Dowager’s Hump,” and how coughing affects the pelvic floor.

The Coughing Affect
Repetitive forceful, quick contractions lead to muscle pain and fatigue. Metabolic effects on fatigued muscles impair muscle function, and neural factors and communication with the central nervous system can impair muscles. The many forceful contractions of a severe cough can cause micro-tears in the muscles, leading to more pain and inflammation.
In manual therapy, we are thinking of inflammation as a “liquid” experience. Inflammation takes up space and irritates nerve endings. Nervous tissue needs constant blood flow to stay alive and healthy. Nervous system fibers that are being irritated by the cells of inflammation, or not receiving blood flow, send out pain signals. An example of this happening in the body can be seen in the pelvic floor. Chronically restricted pelvic floor muscles can lead to nervous tissue dying off around the bladder. Women experience this as pain in the bladder, when really the pain is in the nervous tissue around the bladder. As the pelvic floor muscles release, and blood flow returns to the nervous tissue, the tissue heals, and the pain cycle ends.
Also in manual therapy, when we think of muscle imbalances, we think of some muscles overworking and other muscles underworking. And muscles that are being overworked will eventually “burn out." These muscles will either send pain signals, or they will cause other muscles to take over, which then send out pain signals.
After a muscle performs repeated forceful contractions, it is supposed to rest. You do a leg workout and then you stop. The lungs, though, are always working. Therefore, the muscles of inspiration and exhalation are always working. When someone is coughing for days on end, or has chronic trouble with asthma or GERD, the lungs and the surrounding muscles and fascia are being challenged with additional force but not ever coming to a full rest. This creates an uncomfortable reality.
Chronic conditions lead to other chronic conditions. If someone has a respiratory illness that leads to chronically tight scalene muscles, certainly mixed with other forward head activities ("tech neck"), the shape of the cervical spine will change. Furthermore, forward head posture then stresses the ribcage. Mixed with lung distress, there is a lot to work through.
One final thought: right out of school, I studied a little visceral manipulation, not something I currently practice. But I learned then that the organs have their own plane of rotation. As an example, the diaphragm affects the kidneys; the kidneys move up and down with the diaphragm. Specifically, I remember feeling the ligaments that surround the liver, gently holding space for the liver as it seemed to find a greater place of ease.
As do chiropractors report better visceral function with spinal manipulation, soft tissue therapists believe that the fascia and muscles that surround organs affect the health of the organs. Doesn't this make a ton of sense?
I point all this out so we can think of the body as dynamic and connected. We are trained to think of the body as separate. But it is not. Coughing can create the need for you to repair a stressed muscle, and that is especially likely when mixed with other causative factors, such as daily posture habits.
And—this is crucial—how our body is shaped—how the neck impacts the ribcage and so on—affects our organs and our ability to respond to additional stressors, such as a nasty cough.

A Quick Note About GERD and Coughing
Acid flowing up from the stomach and into the esophagus irritates the throat. An irritated throat triggers a cough reflex. The body wants to clear the throat of any irritant. Someone suffering from GERD can develop a chronic cough, a sore throat, hoarseness, or even difficulty swallowing.
In my practice, I see a lot of women with myofascial sensitivity, GERD, and anterior neck and throat pain. Tension when swallowing has different causes, not just GERD.
The Muscles Involved in Coughing
*Please scroll below for more detailed information on each muscle.
TMJ and Jaw Muscles
Diaphragm
Internal intercostal muscles
External intercostal muscles
Abdominal muscles
Psoas Muscle
Scalene muscles
Sternocleidomastoid muscles
Pelvic Floor Muscles
There are other muscles that have minor actions involved in breathing that are not on this list. And consider: if an illness or muscle imbalance affects the ribcage, it affects muscles not on this list such as the pectoralis muscles (chest muscles).
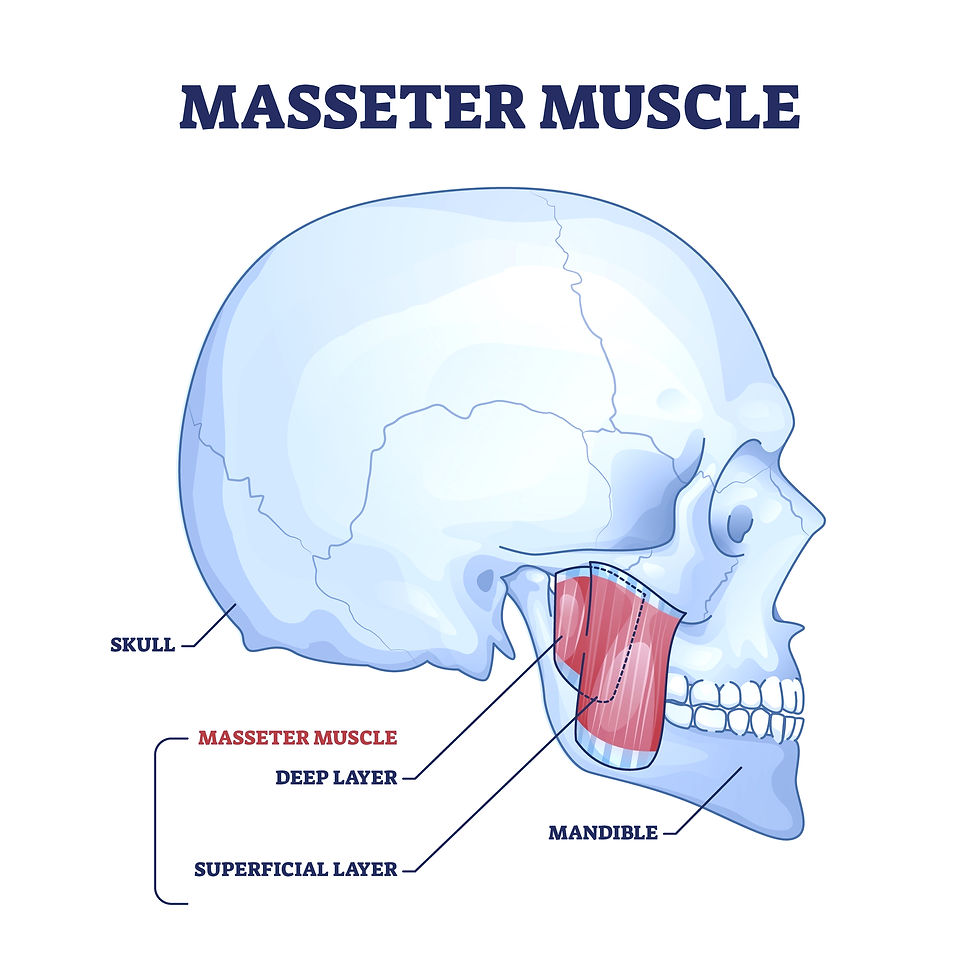
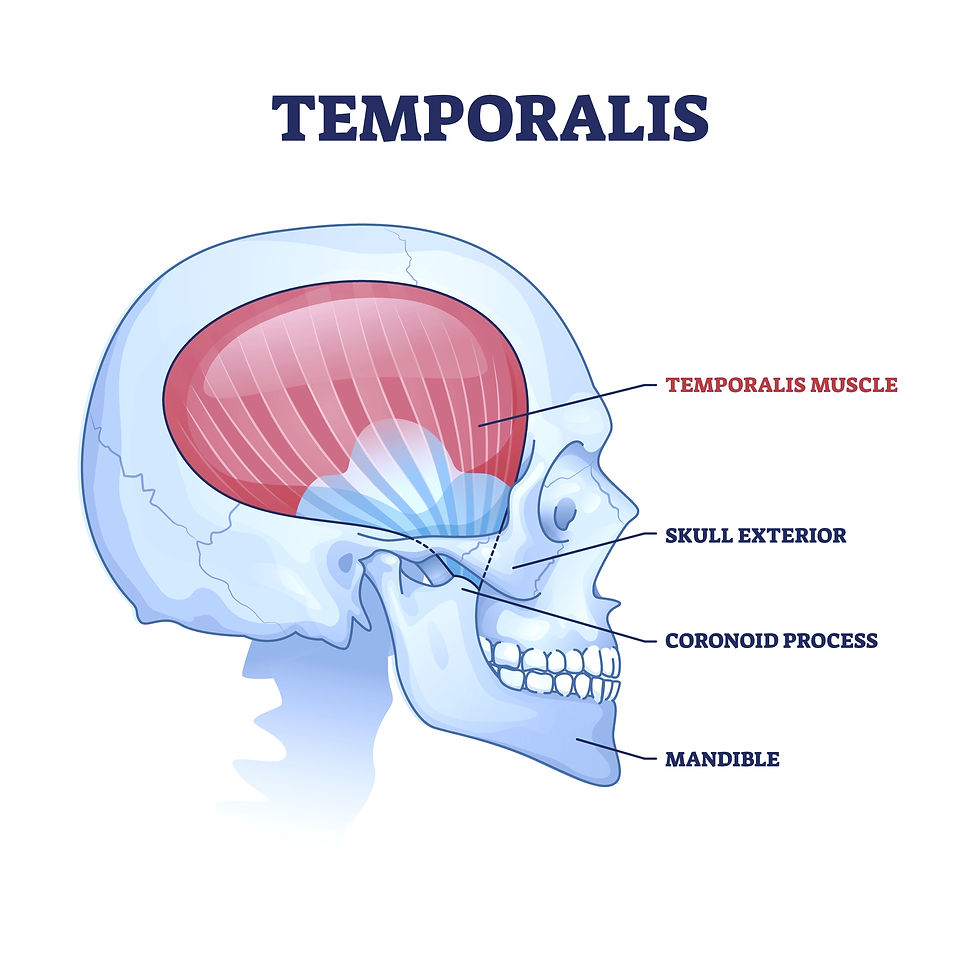
How does coughing affect the TMJ and entire jaw?
As you will read in the scalene muscle section below, coughing places stress on the muscles that affect the cervical spine. Overtime, if that tension is not corrected, degenerative changes will occur. The health of the neck directly affects the TMJ (temporomandibular joint) and the whole jaw.
Since you are connected: if you have GERD and therefore throat irritation, or asthma and/or another illness, and you experience a terrible coughing fit, there can be stress on the diaphragm and psoas—as you will read about below. The stress happening directly to the TMJ and entire jaw affects the TMJ and entire jaw. But the stress of the rest of the body also affects the TMJ and entire jaw.
This is not to overwhelm! You simply investiagte and mindfully notice. Choose something such as your neck or ribcage and apply therapy (with at-home or in-office care). Notice as things feel better and repeat. Because you are connected, several therapies, like intentional breathing or gently stretching the scalene muscles, will help your complete structure. And in the same way, a single powerful therapy will affect many parts of your One Self.
The jaw muscles are not muscles that help to expel air from the lungs, as happens when we cough, but they are working to expel air from the mouth, the exit.
Not only are the TMJ and jaw affected by the neck muscles, the muscles of the ribcage, the psoas, the pelvic floor, and so on, but the jaw is doing its own work. The jaw is moving when you cough, repeatedly opening during inhalation and rapidly closing during the cough.
Clicking in the TMJ—a muscle imbalance issue—can start for the first time or can worsen because of coughing. When the TMJ is affected, the pelvic floor is affected. They connect and mirror each other. As a jaw and pelvic floor therapist, I am always thinking about the pressure chambers in the body. When there is pressure dysregulation, the top and bottom of the spine are affected.
Trigger points in the masseter refer to:
Around the eye and eyebrow, the upper teeth, and the side of the chin.
Trigger points in the temporalis refer to:
Above the eye, the mid-temple, the back of the head, and the upper teeth.
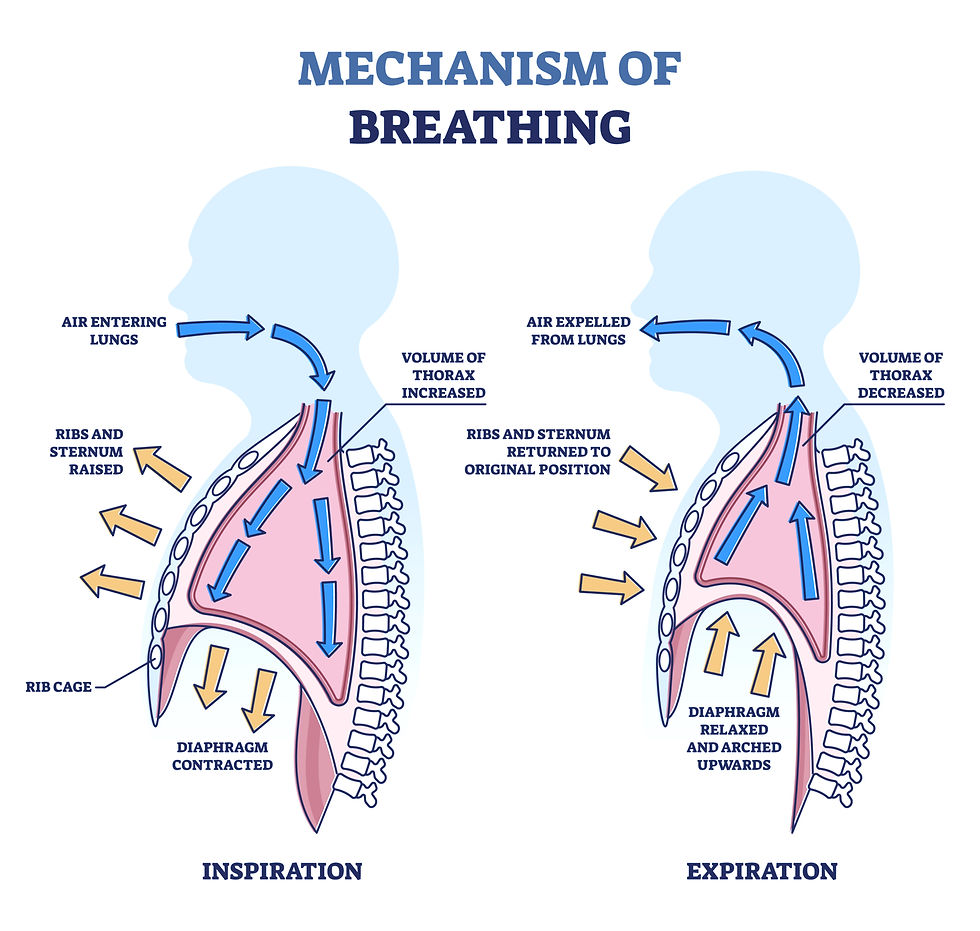
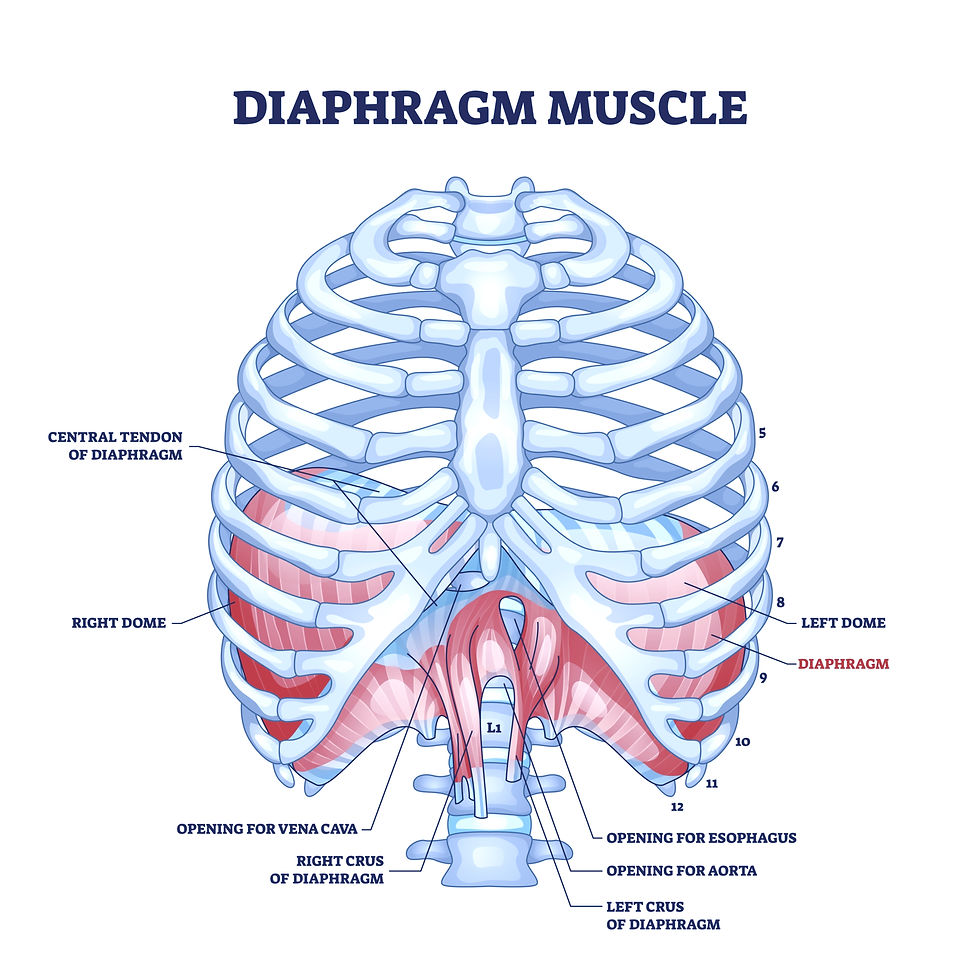
Coughing and the Diaphragm
The diaphragm is powerful, touching every-single-part of our health, and yet it is almost a completely forgotten muscle. We never think of it, and if we do, we think of it as just some muscle that describes breathing. Some of us know it moves down with the breath, but almost no one knows that direct hands-on therapy can affect it; you can feel and affect its edges with your fingertips (more on that HERE—COMING SOON!).
Your diaphragm, described as a “sheet of muscle,” resides inside the thoracic cavity, nestled in the ribcage. The diaphragm inserts onto the back of the xiphoid process (bottom of the sternum), the ribcage (ribs 7-12), and the first couple lumbar (low back) vertebrae (L-1 to L-3). The muscle is unique in several ways, one being that it inserts onto its own central tendon.
Another way the diaphragm is unique is that it is under both conscious and unconscious control. It automatically coordiantes with the lungs, but we can also choose to move it. This happens as you decide to breathe slowly, inhale slowly controlling the diaphragm, and then allow it to drift back up exhaling under conscious control. Our breath moves back up and out under unconscious and conscious control.
Because a cough is repetitive, forceful, and even sometimes “violent,” the diaphragm—like other tissues in the body—can become stressed. To perform a cough, the diaphragm powerfully contracts, expelling air from the lungs.
Notice its connections to the ribcage and low back. And think of all the fascia connections—such as to the psoas, which we will discuss in the psoas description below—that are influenced by the health of the diaphragm.
Muscle imbalances are happening locally, local inflammation, fascia restrictions, pull and pain. But muscle imbalance is also happening in the brain. The brain has trouble coordinating movements of a muscle. Reconnection to the diaphragm can happen by phsycailly working with it and the surrounding muscles, both by a direct touch of a manual therapist, and through your own actions—your own touch and physical work on a yoga mat (again post coming soon), and also through consciously working on the breath to relive tension.
Trigger points in the diaphragm refer to:
Pain around both lobes and up towards the sternum.
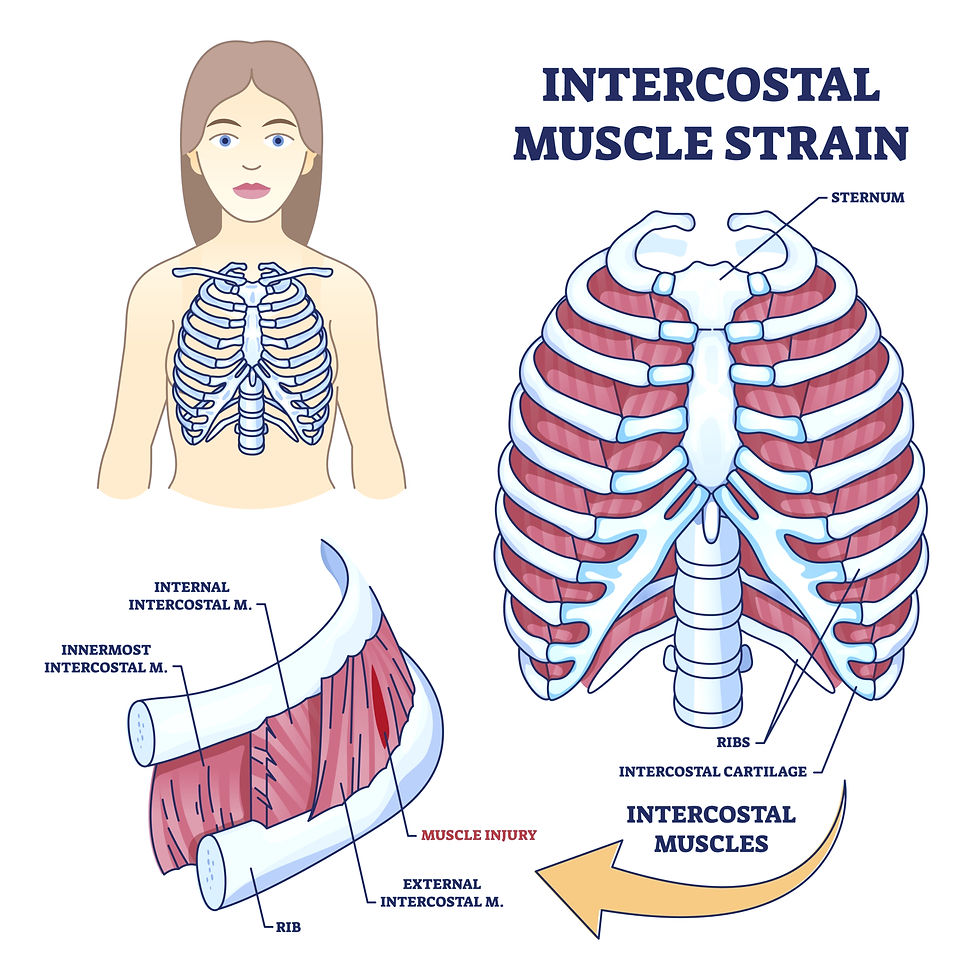
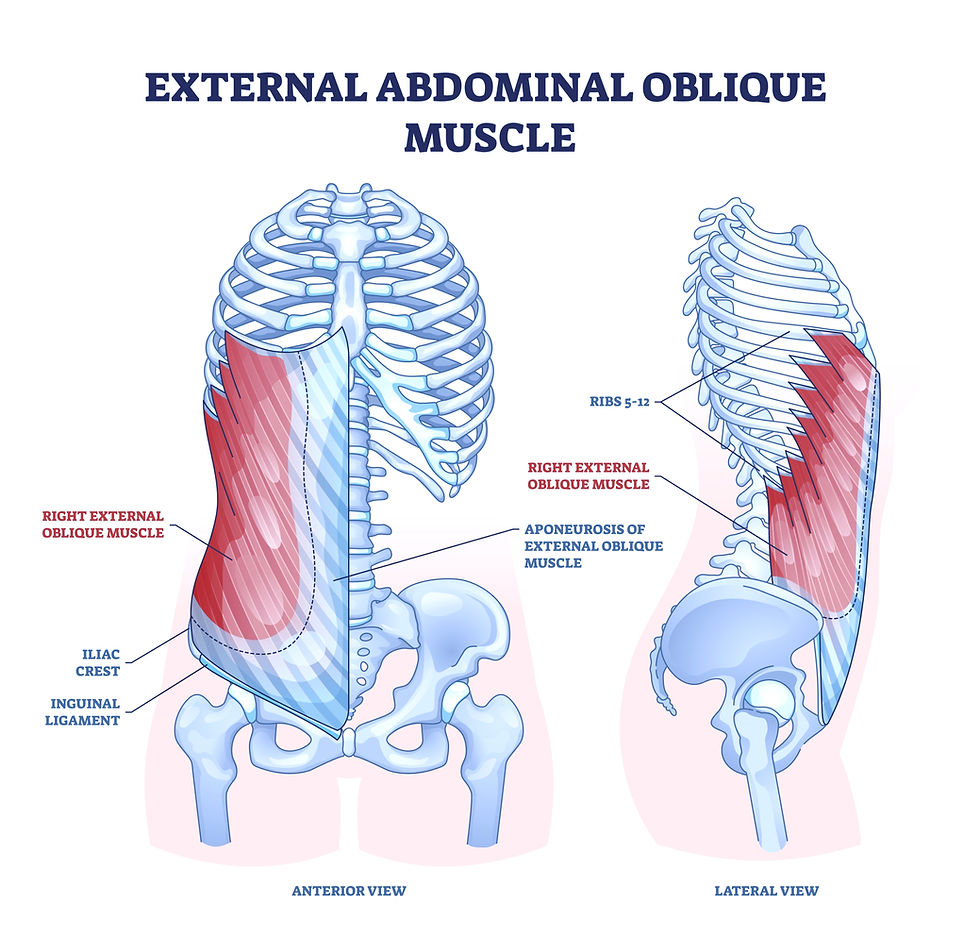
Coughing and the External Intercostal and Internal Intercostals muscles
You have two layers of intercostal muscles, and coughing excessively can strain these muscles. A muscle strain can be a micro-tear or an overstretch.
The external intercostal muscles are thin, flat muscles and are located superficially on the ribcage. Superficial means closer to the surface, the closet ones to palpation.They insert obliquely and originate from the bottom of one rib (a single rib) and insert on top of the rib below. These muscles are between the ribs (1-11) and named as a group. But they are single muscles. One can be sorer than the other.
When you inhale, the external intercostal muscles contract, lifting the ribcage and the sternum upwards and outwards. This expands the ribcage and lowers the lung pressure. The lungs move downward, allowing for a deep breath. They work automatically with the diaphragm. They are active when you sleep and during any type of forceful breathing, such as during exercise. When you exhale, the external intercostal muscles relax and then the ribcage moves the opposite way, down and in.
The internal intercostal muscles are also thin and flat and are deeper, behind the external, and located on the surfaces between the ribs. Like the external intercostals, there are 11 in number, on each side of the ribcage.
When the internal intercostal muscles contract, they pull the ribcage downward and inward. This action expels air from the lungs by reducing the volume of the thoracic cavity. These costal muscles do not contribute during soft, normal breathing; they are recruited during forceful exhalation. They help you cough by firing rapidly , quickly reducing the space inside the thoracic cavity. They work in conjunction with the diaphragm and the external intercostal muscles.
Chest pain: Strained intercostal muscles and strained ribs can cause pain in the chest. Just recently, I worked with a woman who had been to MANY doctors and specialists and had many tests performed that could not explain her pain. She had pain in her chest and could not fully take a breath. No one explained to her that this could have a simple cause, and so she felt quite anxious about her health. Finally, she went to the PT her insurance paid for, but even there they only gave her a pectoralis stretch, without a genuine explanation, and the issue did not resolve. When we worked together, she felt better simply having her body mechanics explained to her. And the worst of her pain, a strained rib and diaphragm... neither of which was that challenging to correct. If you have chest pain, yes, please have it checked out by a doctor, but know that in this system, muscle pain is often misunderstood.
Let’s also note that strained pectoral muscles will also cause local chest pain.
Trigger points in the external and internal intercostals refer to:
External: Local pain, abdominal pain ,and chest pain. Can refer to the groin, testicular and bladder region.
Internal: Local pain, radiating around front of abdomen and down towards the pubic bones.
Quick note: There are also intercostal muscles called the “Innermost.” They are the deepest layer.
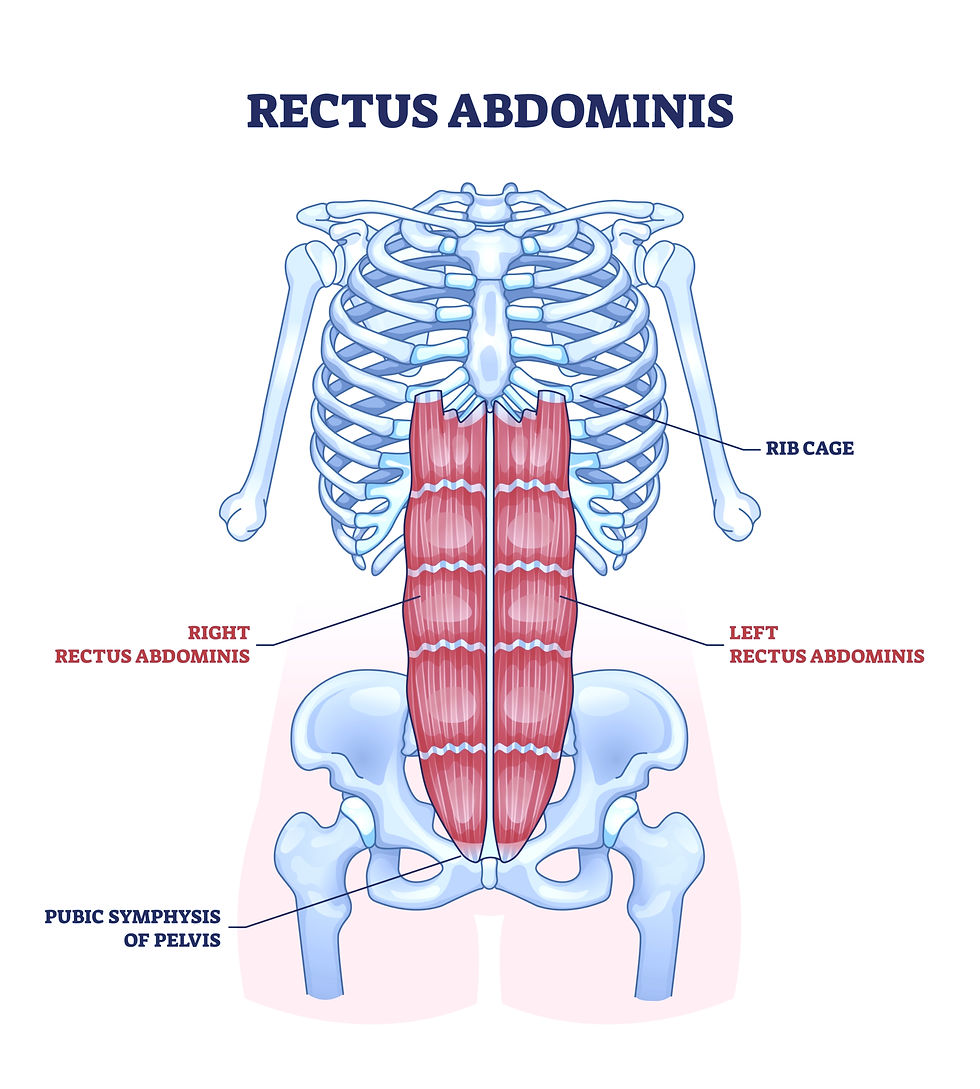
*not shown above are your transverse abs.
Coughing and the Abdominal Muscles
During a cough, the abdominal muscles forcefully contract, helping the diaphragm move upwards, and expelling air. The rectus abdominis contracts and assists air in moving back out. The oblique muscles work hard to stabilize your torso and also assist in contraction.
A forceful contraction pulls at attachment sites. Like all the other muscles, they are subject to stress. Forceful coughing can irritate these muscles and the fascia that surrounds them. Coughing can also aggravate older injury sites. Prolonged coughing, prolonged force, can create strain in the abdominal muscles.
Trigger points in the abdominal muscles refer to:
Abdominal muscle trigger points can refer pain locally across the abdomen. They can also refer pain into the groin, around the bladder, and even horizontally across the mid back.
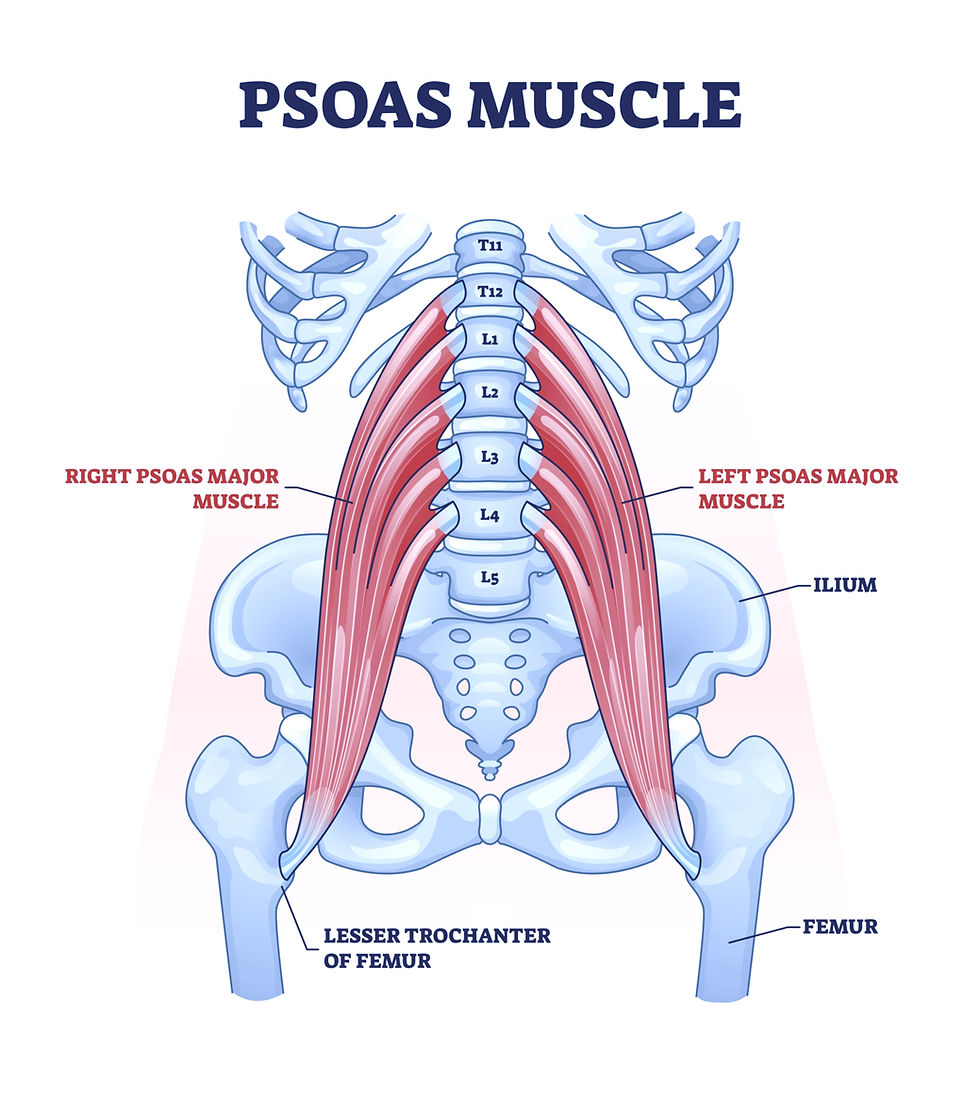
Coughing and the Psoas
Like the other muscles, when you cough, the psoas acts to stabilize the body and aids your core in forcefully expelling air. The psoas and the diaphragm tendons are connected through their attchment sites to the lumbar vertebrae on the anterior spine. The diaphragm's attaches to L1-L3 or L4 (L stands for lumbar) and the psoas runs from T-12 to L5 (T stands for thoracic).
The diaphragm tendon passes over the psoas as it attaches to the spine. All the fascia surrounding the muscles connects them.
Chronically tight psoas muscles lead to postural changes and imbalances that can affect every part of your body, including increased trouble breathing (and even digestion!). A tight psoas can even restrict the diaphragm’s range, which may cause someone to feel unable to take a deep inhale. A shortened psoas will shorten the abdominal wall and the space everything around it has.
Again, like the other muscles, a stressed psoas under the conditions of a chronic cough, or even just an episode of intense coughing, will try its best to meet the extra force required, but the demands can cause additional restrictions and inflammation.
Trigger points in the psoas refer to:
Strong pain in the lumbar spine. And pain from the liiac crest and into the anterior thigh.
Coughing and the Scalene Muscles
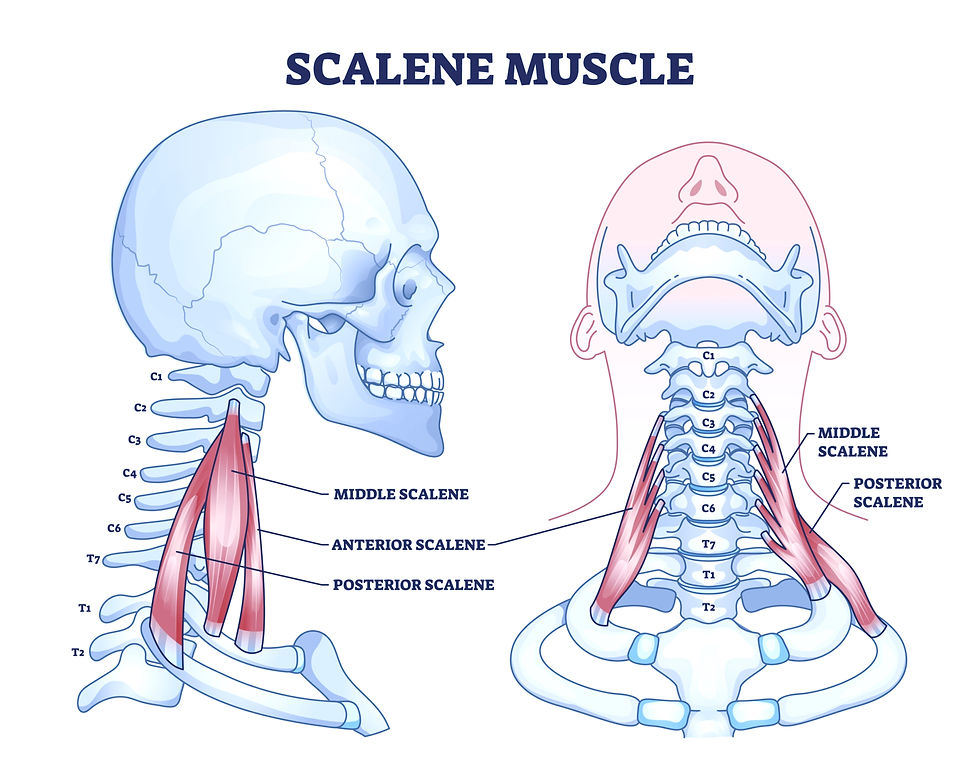
There are three scalene muscles on each side of the neck. Scalene muscles are attached to the neck and the first two ribs. During inhalation, they assist in lifting the first two ribs. This elevation of the ribcage facilities deeper breathing.
In my TMJ and neck practice, I talk to women about how shallow breathing affects these muscles. Since these muscles are assisting in the ribcage's elevation, when you take short quick breaths, these muscles are working harder than they should. Long and slow breaths allow them to lengthen and rest.
During a cough, the scalene muscles forcefully contract to stabilize the neck and to lift the ribcage.
Because of poor posture, computer neck “tech neck,” and looking down at a phone, these muscles are often already hypertonic, holding way too much tone and tension. Chronically tight scalene muscles draw the cervical spine forward, stressing the back of the neck and shoulders and the jaw above. Chronically tight scalene muscles lead to degenerative changes in the spine. If these muscles are already an issue, and then you squeeze them harder during repeated coughing episodes, their tension will increase. After an illness, some of that tension may drop on its own, but your body is also very likely to hold on to some tension, adding to the tension you already have.
Scalene muscle dysfunction is a major reason women have neck and jaw pain.
Trigger points in the scalene muscles refer to:
Front and back of the arm to the thumb and index finger. On the back, the upper part of the scapula and on the front chest, into the pectorials muscle and towards the nipple.
Read more about the scalene muscles HERE
Coughing and the SCM
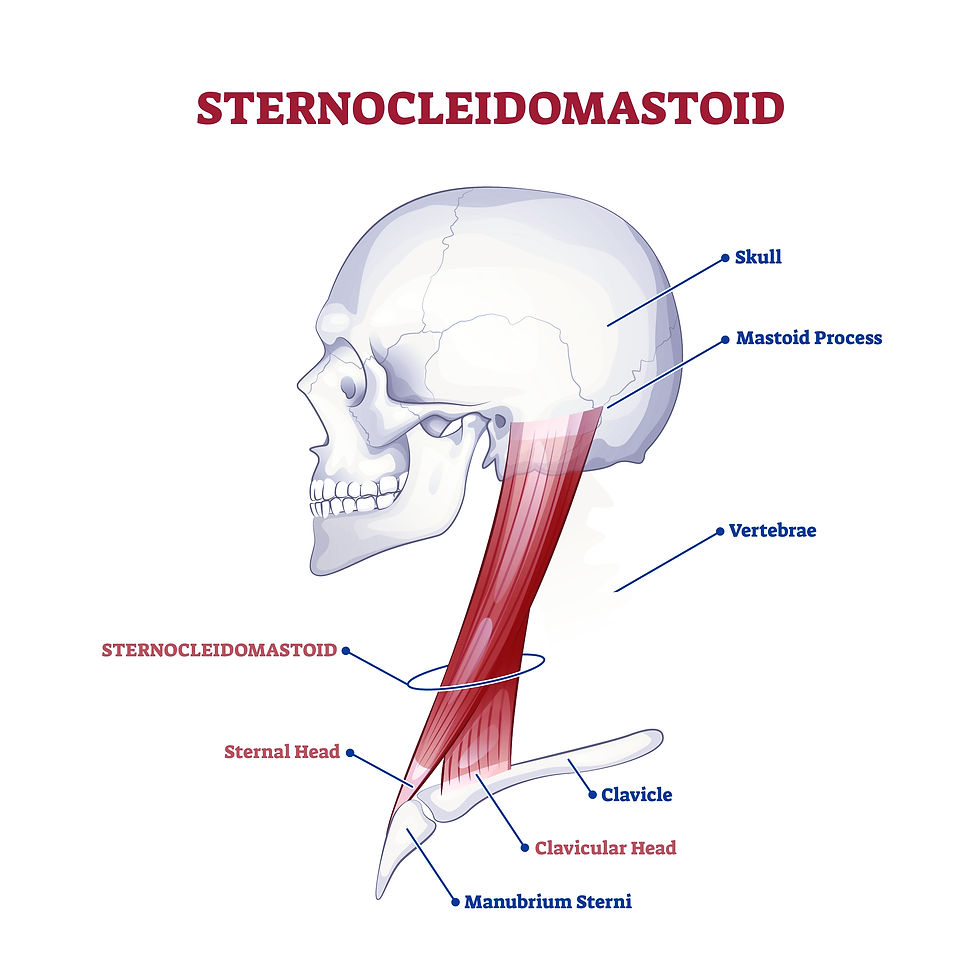
Also on the anterior neck, a dysfunctional SCM muscle causes a large variety of symptoms.
Many of these symptoms caused by a dysfunctional SCM muscle send women searching from doctor to doctor, never finding answers. But if you know about these muscles, the mystery is not mysterious at all.
While the scalene muscles aid in quiet, restful breathing, and active breathing, the SCM mainly gets recruited—for breathing—during an active, forceful breath.
During a cough, these muscles are forcefully assisting in the ribcage’s and chest's elevation, by pulling up on the clavicles. The vagus nerve—which innervates (among other things) the lungs and the heart—runs directly behind the SCM.
The health of the SCM affects the health of the vagus nerve. The health of the vagus nerve affects the lungs.
Slumping and even limping affect the SCM. Forward head posture is incredibly stressful to these muscles, which can send pain signals to the jaw, the back of the head, behind and inside the ear.
Trigger points in the SCM refer pain to:
The back of the head, the occiput, the eyebrows, the cheek, the throat, and can mask as headaches, earaches, and mastoid pain.
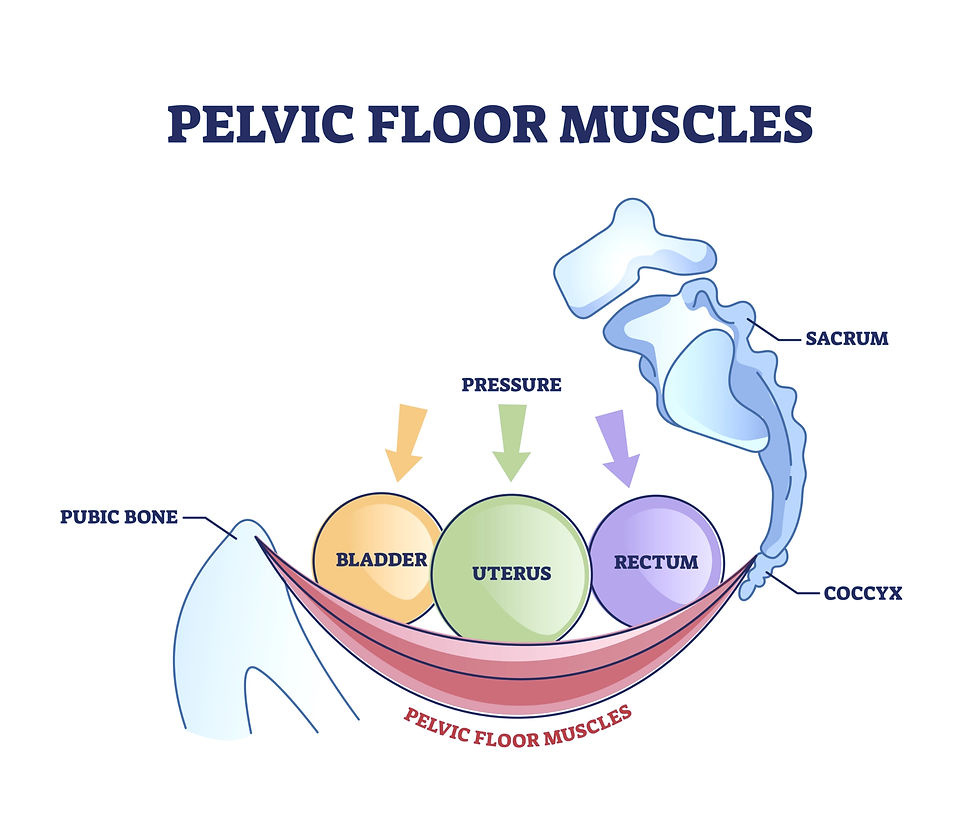
Coughing and the Pelvic Floor
Coughing creates a sudden increase in intra-abdominal pressure, and the pelvic floor, a group of core muscles, responds. When you cough, a healthy pelvic floor moves, protecting the bladder and other organs. It works in coordination with the diaphragm.
The image of a balloon is frequently used. If you squeeze the top of a balloon, you will see the bottom of the balloon expand. When pressure increases above the pelvic floor, it should expand and slightly lengthen out to accommodate that pressure, and then in coordination with the other core muscles, as the pressure in the above chambers decreases, the pelvic floor rises back up. The expansion downwards is on the inhale, and the rise back up is on the exhale. Everything in your core expands and then everything in your core comes back to center. In the moments between, the pelvic floor is buoyant. Strong and holding space but not overly tight and overworking.
Bladder leakage during a cough happens because the pelvic floor muscles are 1) not strong enough to hold against the pressure of the above force 2) the pelvic floor muscles are too tight and already creating nervous tissue and organ stress (OFTEN the case) 3) the muscles are a mixture of weak and tight. It is worth noting here that chronic tension eventually leads to weakness. 4) the pelvic floor muscles cannot coordinate with the other core muscles. They are not rising and falling as they should, even during a normal breath.
Since a cough is a sudden force, a stressed pelvic floor will be more stressed and the dysfunction, the lack of coordination, will be more prominent. Long-term pelvic floor health is about learning what your muscles need and intentionally learning to coordinate the movement of these muscles so that they are then better able to perform under subconscious control—at the moment of a sneeze or cough.
Trigger points in the pelvic floor can refer to:
Tailbone, low back, hip, and the groin.
Tips for protecting your pelvic floor during a cough can be found HERE (post coming soon!)
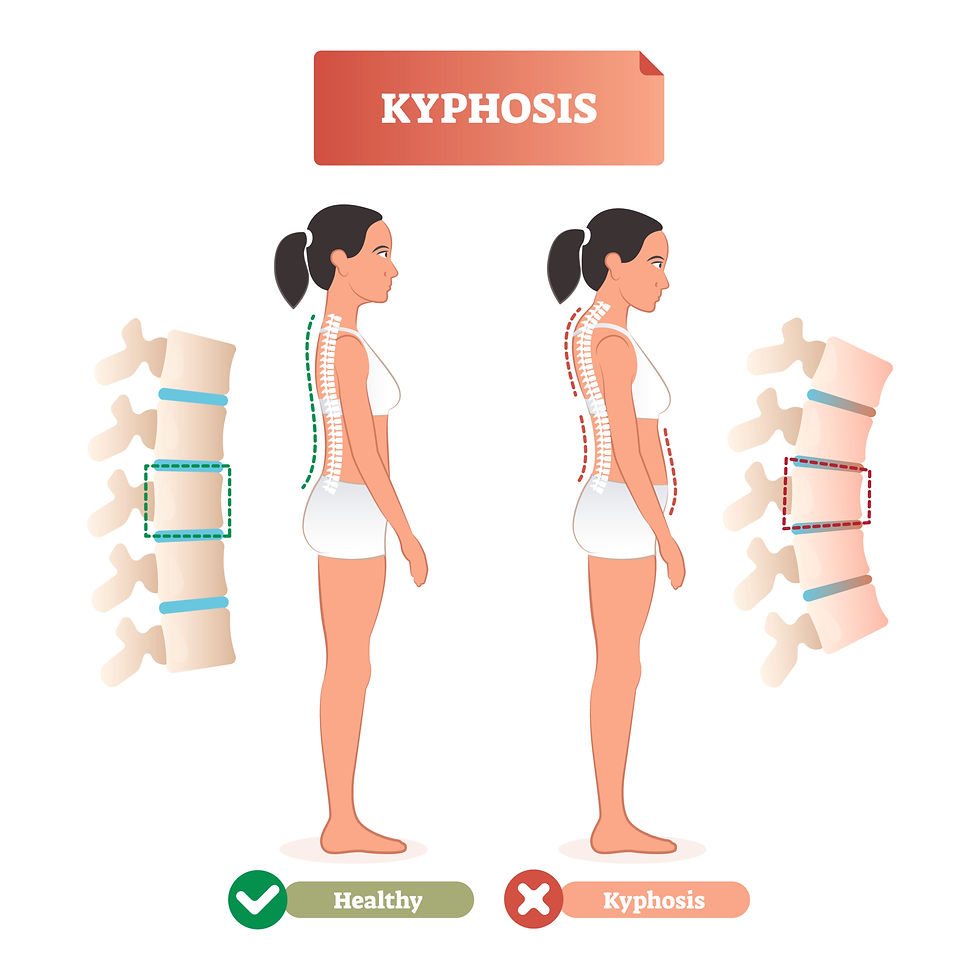
Chronic Coughing and Dowager's Hump
Chronic coughing causes chronic tension and hard scalene muscles. This causes degenerative changes in the spine. As the hypertonic scalene muscles pull the neck forward, the ribcage sinks back. Over time, degenerative changes happen in the cervical spine and the thoracic spine. Kyphosis is an excessive outward curvature of the thoracic spine. It happens in varying degrees, and many women need to work actively on healing this posture. Dowanger’s hump seems a little more severe, is associated with fatty tissue around the curve at the bottom of the neck and top of the thoracic spine, and in older age, can be associated with osteoporosis. As the spine degenerates, the neck and head experience increased stress, leading to a higher risk of tripping, falling, and head injuries.
To prevent this cascade, women with respiratory illnesses should receive physical medicine. Certainly, to help heal, understanding mechanics and your body’s respiratory distress is essential.
Summing it Up
If you have a chronic cough or GERD, or even if you have just a momentary respiratory illness, the above muscles can be affected. Because of trigger points, pain from the psoas can radiate into the bladder. Stressed pelvic floor muscles can directly irritate the bladder. Your body is connected.
Don’t be overwhelmed. Use this post to investigate your emotional and physical symptoms. Choose a muscle such as the scalene muscles, and work on developing a healing relationship with it. Notice the changes. And then add to your program.
Want to Know More?
I have more posts coming soon,. Stay tuned!
Check out my books on health and wellness!

The Elemental Woman
A Conversation for the Modern Western Woman Inspired by the Healing Wisdom of the Ancient Eastern Sage

Food & Mood Journal
A tracking guide to connect the food you eat, the emotions you feel, and increase the feeling of deep self-love

Mindful Movement Journal
A tracking guide to connect the motions you make, the emotions you feel, and increase the feeling of deep self-love
Basic Ayurveda
The Elemental Woman Supplement Guide
About the author:
Since 2004, Tara Lee Clasen has been assisting women on their healing adventures. As a woman-focused physical medicine provider, also trained in Eastern medicine, she knows transformation is possible and knows that with reflection and self-love, your future is full of bright possibilities.
#tmjpain #tmj #neckpain #shoulderpain #ribpain #chronicpain #jawpain #headaches #migraine #whiplash #asthma #vagusnerve #massagetherapy #manualtherapy #chiropratic #tmjpain #tmj #neckpain #shoulderpain #ribpain #chronicpain #jawpain #headaches #migraine #whiplash #asthma #vagusnerve #massagetherapy #manualtherapy #chiropratic
LINKS:









Comments